FAQ
Answers to commonly asked questions about dental network participation.

How do I become a participating provider?
The Join our network page includes a checklist of what you need to have on hand when you apply and a link to the application.
Who is my dental network manager?
Our dental network managers are available to answer your questions and support you and your staff. Each state has a designated dental network manager. You can find your dental network manager on our provider website at the Contact us page.
How can I verify my patients’ benefits and eligibility?
You can find patient information and process claims reimbursement quickly and easily through MyDentalCoverage. For FEP dental members, you will need to use Availity Essentials to check benefits and eligibility.
How do pre-determinations work?
The patient cost estimator is no longer available on Availity for dental business, for cost estimations for non-transitioned members please file a pre-determination on Availity Essentials. All other members submit pre-determinations on MyDentalCoverage or use the online cost estimator.
Benefits will be predetermined under the assumption that Regence is the primary insurer. If the patient is insured under more than one policy, actual benefits payable may be adjusted due to coordination of benefits (COB) or maintenance (non-duplication) of benefits (MOB).
Predeterminations are provided as a courtesy and are not a guarantee of payment. All services are subject to the benefits, eligibility and maximum allowable amounts in effect on the actual date of service. Estimated payment may be reduced due to prior payments for treatment. Actual benefits payable will depend upon the following:
Benefits available
Member contract limitations
Provider participating status
Patient and provider eligibility
Benefit maximums in effect when the services are completed
How do I estimate member costs?
The cost estimator is no longer available in Availity. To receive estimated costs you will need to submit a pre-determination through the Availity portal. For a member who has transitioned to the new platform, please visit MyDentalCoverage.com.
Where can I find a reimbursement schedule?
Reimbursement schedules and pricing tools are available at our online portal, Availity Essentials.
How do I register for Availity?
Create an account at Availity Essentials. For technical support, please call 1-800-282-4548.
Who do I contact if I need 1099 form assistance?
If you need assistance with your 1099, please call 1-866-445-5148 toll-free. You’ll be connected to an automated answering system that can answer all commonly asked questions 24/7. You can also speak with a live representative during business hours if you need additional assistance.
What if I still need help?
You can find the number of a representative who can help you on our Contact us page.
What is Dental4Health?
Regence’s Dental4Health® program is designed to help members with certain medical conditions affected by oral health maintain a healthy mouth—and body. Enrolled members receive additional dental benefits at no cost, including preventive and periodontal services, outreach and education, and specialized medical care programs. They have no out-of-pocket costs or waiting periods, and the benefits don’t apply toward their plan’s annual maximum.
What medical conditions are included in the program?
Chronic obstructive pulmonary disease (COPD)
Coronary artery disease (CAD)
Diabetes (DM)
End-stage renal disease (ESRD)
Metabolic syndrome (MetS)
Oral, head and neck cancers (OC and HNC)
Pregnancy (PG) (members who are currently pregnant)
Sjögren’s syndrome (SjS)
Stroke (CVA)
What dental services are included in the program?
Program services can be viewed in this table.
How can my patients enroll in Dental4Health?
Members who have a Regence medical and dental plan and who have been diagnosed with one or more eligible conditions are automatically enrolled.
Members who only have a Regence dental plan can submit a paper enrollment form found on regencedental.com.
How can I find out if a patient is already enrolled?
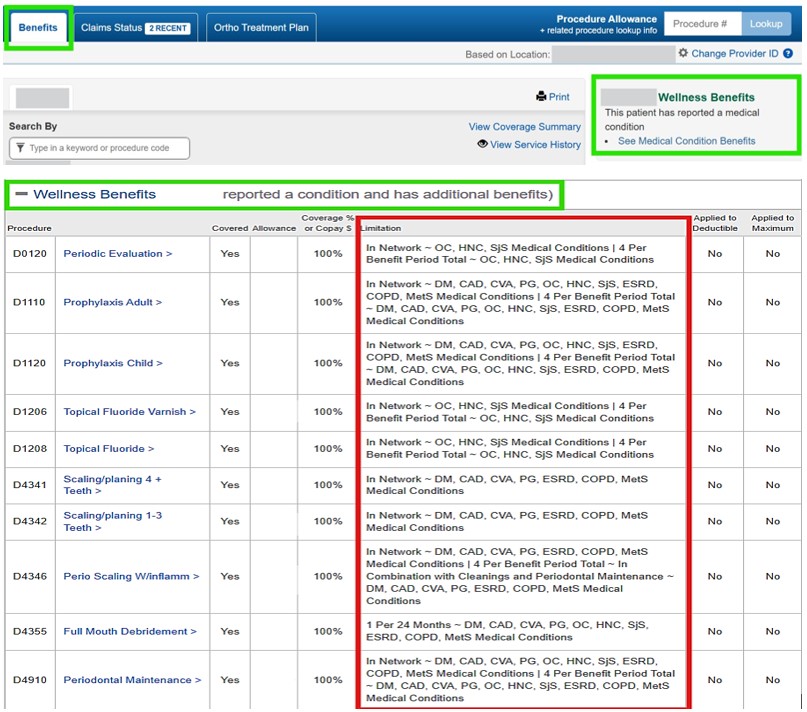
You can confirm your patient is enrolled in Dental4Health by logging on to MyDentalCoverage. To verify a member’s eligibility and status:
1) Search for your patient by member ID and date of birth.
2) Once in the patient profile, select the Benefits tab.
3) If a patient is enrolled, the Wellness Benefits box on the right-hand side will indicate, “This patient has reported a condition.” Then, the section will expand to display which benefits are covered and for which conditions (see example below).
You will need to confirm with the patient which condition(s) made them eligible for enrollment.
Where can I learn more about the Dental4Health program?
You can find more information about the program by reviewing the providers' guide to Dental4Health on our website or by contacting your Regence dental network manager.